Unlocking the Power of Proteins
Chemistry of Life Processes Institute (CLP) at Northwestern University is pioneering the greatest wave of biomedical innovation since the Human Genome Project opened the door for individualized medicine two decades ago. Known as proteomics, this fast-growing field identifies and measures the various forms of proteins (proteoforms) that link genes and disease in order to diagnose and treat threats to human health.
CLP houses the premier center for proteomics under the leadership of Neil Kelleher, a leading advocate for the Human Proteoform Project, a global initiative to map all proteins in the human body. Leveraging an unsurpassed capability to analyze proteins, the Institute is ready to launch the next era of precision medicine by discovering the changes in proteoforms that cause disease, creating sensitive diagnostics to catch disease early and prevent organ damage, and identifying new, proteoform-enabled targets for drug development and delivery.
Through its Convergence Research Initiatives, CLP assembles world-class teams of Northwestern chemists, clinicians, life scientists and engineers to transform how we diagnose, treat and, someday, cure devasting diseases that have eluded effective treatments, including liver and pancreatic cancers, Alzheimer’s disease and amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease.
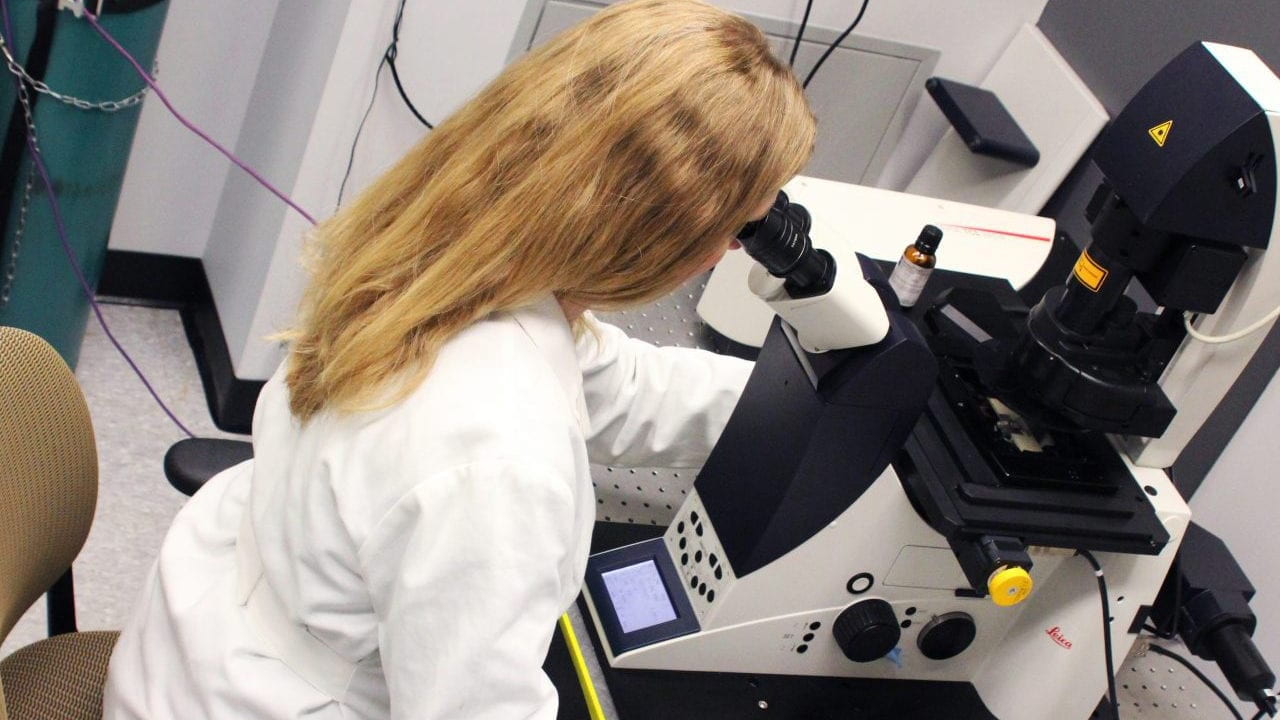
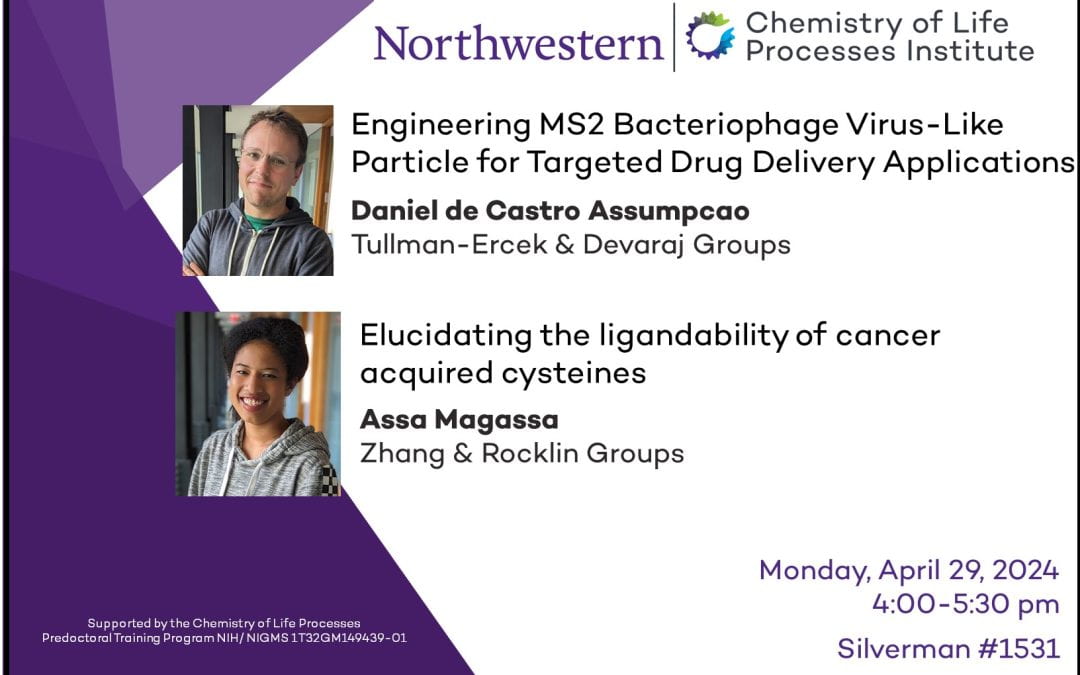
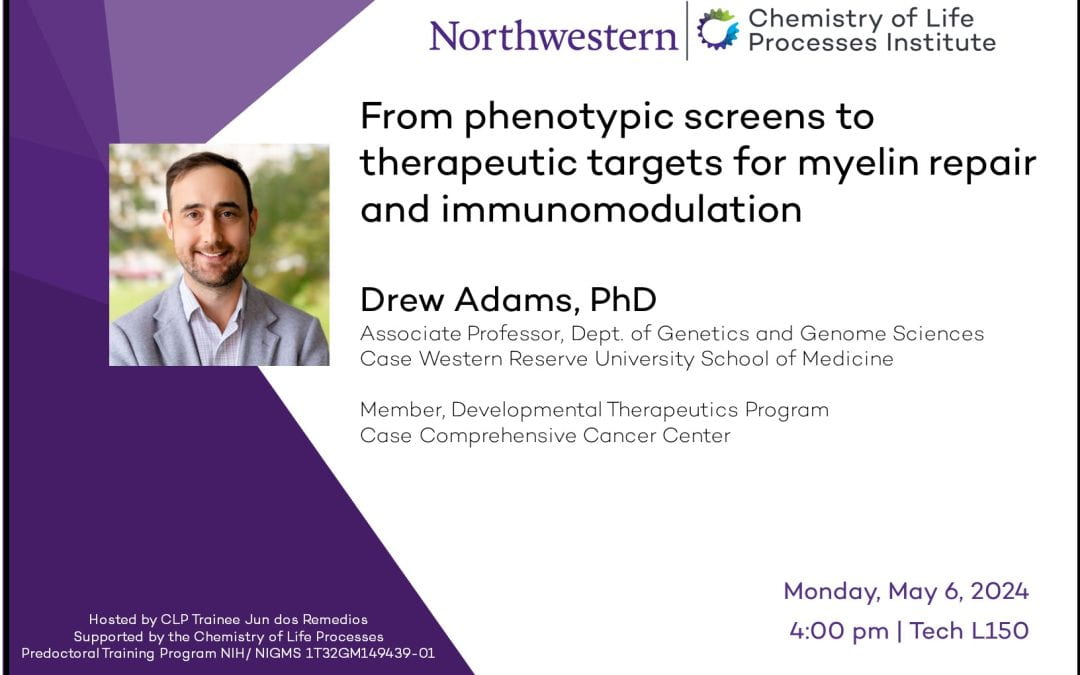
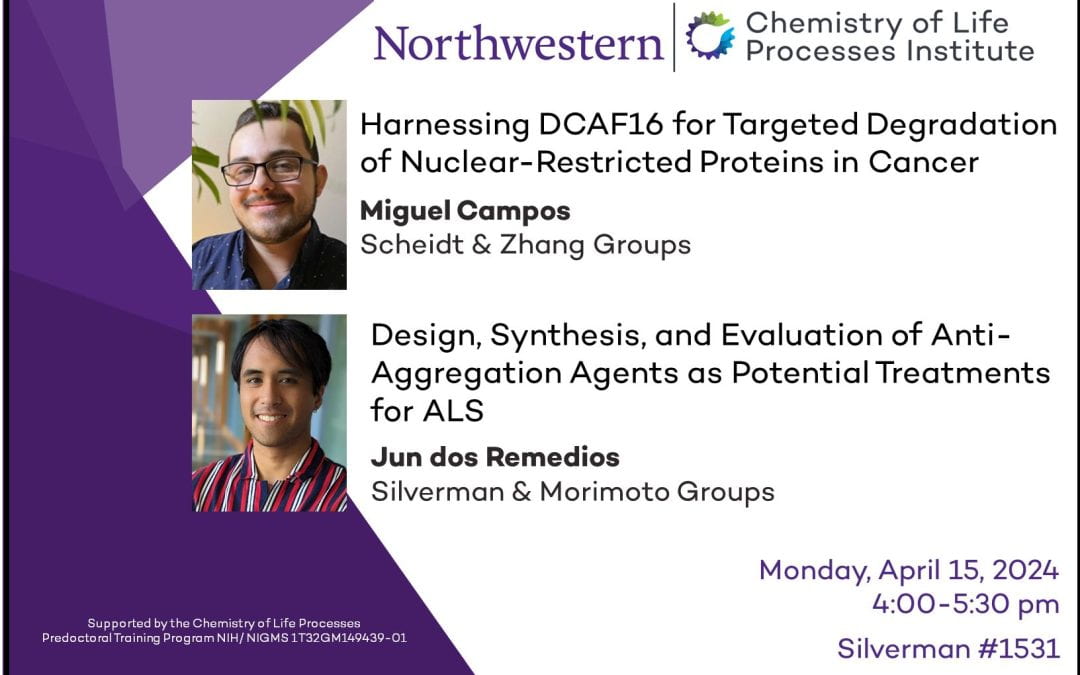
Training the Next Generation of Scientists
CLP’s world-class research and training programs prepare Northwestern undergraduates and graduate students to tackle tomorrow’s biggest biomedical challenges. Students and trainees are required to work with two mentors from different disciplines to learn multiple languages of scientific inquiry. Our curricula emphasize skills development, rigor, reproducibility and hands-on training across a broad spectrum of instruments and methods.
Together with our partners across the University, Northwestern Medicine, and Lurie Cancer Center, we pioneer new science and hasten the delivery of life-changing innovations to society.
“At CLP, mapping the universe of human proteins is already underway, and with donor support, we’ll be able to accelerate the ability to detect human disease earlier and develop precision medicines. We’re powering drug development with truly next generation proteomics.”
Neil L. Kelleher, PhD | Director of CLP
BY THE NUMBERS
INVESTING IN INNOVATION
$1.2M Invested in CLP Institute seed projects
$24M New external funding resulting from seed grants
IN THE PIPELINE
35 New drug candidates
31 Medical devices
9 Diagnostic technologies
BENCH TO SOCIETY
33 New companies spun out by Institute faculty
$2.5B External investments in new companies
Read All News

Northwestern’s Chemistry of Life Processes Institute Receives a Grant Award from The Michael J. Fox Foundation
As is the case with many other diseases, a protein is thought to be a key driver of Parkinson’s disease (PD). Thanks to a two-year $700,000 grant from The Michael J. Fox Foundation for Parkinson’s Research (MJFF), researchers in Northwestern’s Chemistry of Life...

Student Spotlight: Ananya Basu
Ananya Basu, a third-year PhD student, is using innovative approaches to overcome previously intractable targets in the Zhang Lab. Appointed to the CLP Predoctoral Training Program, she is being co-mentored by Zhang (chemistry) and Horvath (molecular biosciences)....
Transfer learning paves the way for new disease treatments
Technological advances in gene sequencing and computing have led to an explosion in the availability of bioinformatic data and processing power, respectively, creating a ripe nexus for artificial intelligence (AI) to design strategies for controlling cell behavior. In...

Neil Kelleher to Headline and Receive Distinguished Contribution Award at US HUPO 2024
Neil Kelleher, Walter and Mary Elizabeth Glass Professor of Chemistry, Molecular Biosciences, and Medicine at Northwestern University, will present his groundbreaking work and insights at US HUPO 2024 in Portland, Oregon next week as the 2024 recipient of the Donald...